by Annika Morse



This podcast explores the intersections of reproductive justice and systemic inequities in postpartum care, focusing on historical and contemporary treatment of postpartum depression (PPD). It discusses the medication Zurzuvae, comparing it’s benefits and shortcomings as a medical advancement.
Transcript
- Hi, my name is Annika and I’ll be your host today. Welcome to Beyond Birth, where we will be discussing an often-overlooked aspect of reproductive justice: the postpartum experience. In this episode, we’ll explore the intersections of identity and systemic challenges that shape the postpartum experience for mothers, narrowing in on treatment of postpartum depression.
- The weeks and months after childbirth, known as the postpartum period, can be a time of deep change. In the time after birth, mothers not only face the demands of caring for a newborn baby, but also the task of caring for themselves as their bodies heal. These drastic changes in responsibilities, routine, relationships, and body can invoke immense shifts in hormones. Women may experience conditions like postpartum depression, or PPD. The National Library of Medicine states that PPD affects “approximately 1 in 7 women within the first year after childbirth,” with up to 50% of cases going undiagnosed. (1)
- The depressive symptoms associated with PPD can be debilitating, and directly correlate with the pillars of reproductive justice. Loretta Ross, a feminist activist, defines reproductive justice as the right to not have a child, the right to have a child, and the right to raise said child in a safe and healthy environment. (CITE 2). Postpartum depression may disturb the third right of RJ, not allowing the mother to raise her child to the best of her ability, and to keep herself and her child safe.
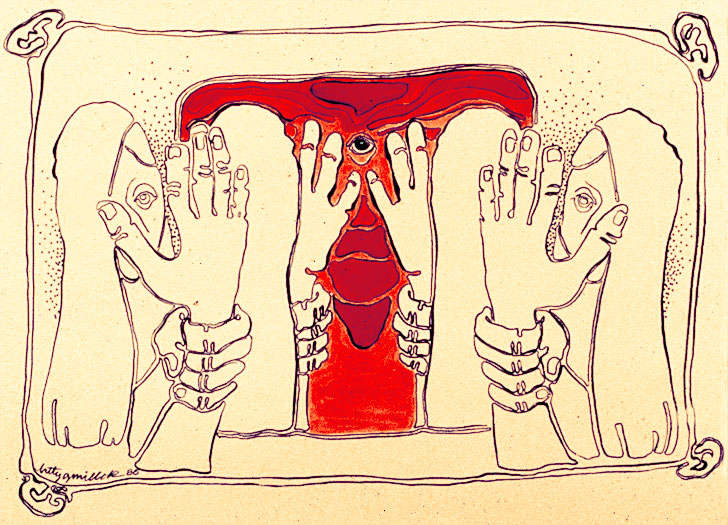
- Despite how common PPD is, the historical response to it has been disappointing. This condition was often dismissed as “baby blues”, a natural phase mothers should simply get over, which diminishes the complex nature of mental health. Treatments like electroshock therapy were common and featured limited regulation. I even have a family friend who’s mother passed away as a result of electroshock therapy for PPD in the 1950s. Stories like these are common, and stigma surrounding postpartum depression is present to this day, illustrated by the diagnosis rate.
- Even as social awareness and medical research on the topic has grown, the medical field has been slow to address postpartum depression in meaningful ways.
- Postpartum care is often fragmented and inconsistent. Medical check-ins with the mother after childbirth are sparse, often limited to a single six-week appointment. Baby takes most of the focus. A research participant from an article, Toward reproductive justice in postpartum care, shared that she “felt like I wasn’t receiving the proper care afterwards, whereas during and directly after [childbirth], like the first two hours after, I was receiving constant care… To go from having a doctor constantly to being moved to… another floor after delivery… bjust having a major surgery, and not having anybody to come check on you, it’s a really horrible feeling.” (3)
- This switch from high to low care after childbirth fails to address multitudes of issues new mothers may experience in the healing process, like PPD. A lack of continued care makes it difficult to address issues as they arise. For individuals from marginalized communities, these challenges are even more pronounced.
- One of the biggest barriers to adequate postpartum care is cost. Low income mothers may not have the chance to take time away from working to heal or seek treatment if they experience symptoms of postpartum depression. In the United States, access to these services are limited by insurance coverage.
- Let’s take a look at a recent development. In August 2023, the Food and Drug Administration approved the first oral medication to treat postpartum depression. Zurzuvae is a pill, providing ease of access. The only other FDA approved treatment specifically for PPD is brexanolone, which costs over $30,000 and requires an IV administered in a medical setting. (4) Some treatments involved antidepressants not tailored for postpartum depression. These SSRIs take longer to kick in than Zurzuvae, which was found to be effective and fast-acting in clinical trials. (5)
- However, the 14-day course of Zurzuvae costs $15,900. In response to this shockingly high price tag, the companies producing the medication state they are working with insurance companies for affordability. (6) The reality is, this won’t be enough for everyone. Many women, particularly those low-income, uninsured, or without comprehensive insurance, won’t be able to access this treatment. Even with insurance, gaps in coverage or co-pays could leave users financially burdened. Criticism for this price point is heightened, considering Zurzuvae serves such a vulnerable facet of the population. But this cost is common in the drug industry – once a new medication is released, costs are high to make back funding spent on development, testing, and approval. Insurance companies prefer to keep clients on cheaper therapies than try new drugs, and will require those to be attempted first before approving a drug like Zurzuvae. Some insurance policies mandate that a psychiatrist must prescribe the drug, rather than an OB/GYN. Many insurers will not pay for a psychiatrist.
- These corporations benefit from the taboo nature of PPD. They are less likely to experience pushback on price for something with such a stigmatized nature. The same mechanisms that make this medication so new – despite the condition existing as long as motherhood has – allow it to be so expensive.
- The postpartum experience is an essential part of the reproductive justice framework. It is not simply about being pregnant and giving birth, but having the chance to recover, heal, and thrive. Access to safe, affordable, and effective treatment of postpartum depression should be a basic right for all mothers under reproductive justice, yet systemic barriers leave many women without the help they need.
- Thank you for listening to this episode. The development of Zurzuvae is a positive step in addressing the need for more specialized treatments for PPD, but it highlights the gap in the reality of access, and the larger issue of healthcare inequality. Its out-of-reach nature fails in providing true reproductive justice.
Sources
1) Carlson, Karen. “Postpartum Depression.” StatPearls [Internet]., August 12, 2024. https://www.ncbi.nlm.nih.gov/books/NBK519070/.
2) Ross, Loretta, and Rickie Solinger. Reproductive Justice: An Introduction. Oakland, CA: University of California Press, 2017.
3) Tully, Kristin P, and Alison M Stuebe. “Foreward: Toward Reproductive Justice in Postpartum Care.” Clinical obstetrics and gynecology, September 1, 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC9339469/.
4) Hassanein, Nada. “There’s a New Pill for Postpartum Depression, but at-Risk Women May Face Difficulties Getting It • Washington State Standard.” Washington State Standard, January 11, 2024. https://washingtonstatestandard.com/2024/01/11/theres-a-new-pill-for-postpartum-depression-but-many-at-risk-women-face-hurdles/.
5) Commissioner, Office of the. “FDA Approves First Oral Treatment for Postpartum Depression.” U.S. Food and Drug Administration. Accessed December 2, 2024. https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-treatment-postpartum-depression.
6) Tanneeru, Manav. “New Postpartum Depression Drug Gets Almost $16,000 Price Tag, Raising Questions about Access.” CNN, November 8, 2023. https://www.cnn.com/2023/11/07/health/postpartum-depression-drug-price-tag/index.html.
7) Britt, Rebecca. “Zurzuvae, the New Postpartum Depression Drug Now Available in the U.S. – This Is How Insurers Have Responded.” Policy Center for Maternal Mental Health, May 2, 2024. https://policycentermmh.org/zurzuvae-the-new-postpartum-depression-drug-now-available-in-the-u-s-this-is-how-insurers-have-responded/.
Image used
8) “Postpartum Depression Drugs Market Size Report, 2030.” Postpartum Depression Drugs Market Size Report, 2030. Accessed December 2, 2024. https://www.grandviewresearch.com/industry-analysis/postpartum-depression-drugs-market-report.
Image used
9) “A Brief History of Electroconvulsive Therapy.” Psychology Today. Accessed December 2, 2024. https://www.psychologytoday.com/intl/blog/freud-fluoxetine/201811/brief-history-electroconvulsive-therapy
Image used