Syd Brown

Many different religions have historically had an impact on the workings of the healthcare system. This podcast episode will focus on Catholicism in health care, specifically the Ethical and Religious Directives that Catholic hospitals and educational institutions must follow, and how these directives have become dangerous to reproductive healthcare.
Transcript
Hello and welcome to Directives and Decisions: Conflicting Medical Guidelines in Catholic Healthcare Systems. This podcast episode will be discussing the contradiction of Ethical and Religious Directives and the program requirements of the medical field when it comes to reproductive care. I’m Syd Brown, and as your host I will walk you through the history of these Ethical and Religious directives, their modern world impact, and how they are negatively affecting patients and medical professionals alike.
So what is an ERD, and where did they come from? Well in 1915, the Catholic Health Association (or the CHA) was founded in response to growing medical technology. The CHA wanted to uphold Catholic beliefs while also providing quality care. In their mission to do this, a list of Ethical and Religious directives (more widely known as ERDs) were created by a combination of theologians and medical professionals to act as guidelines of how to provide proper Catholic healthcare. However, the problem was these directives were seen as more optional guidelines, rather than hard and fast rules. So in 1971, the CHA released an updated version of the ERDs, which would be accepted as official rules in 1973, not so coincidentally lined up with when the original decision of Roe v Wade ruled in favor of protecting a person’s right to have an abortion. The CHA continued to modify the ERDs until the 7th and most recent edition was released in 2025.
The 7th edition of the ERDs includes direct orders against medical procedures relating to abortion, contraception, gender affirming care, and even surrogacy. Directive number 45 states “Procedured abortion (that is, the ‘deliberate and direct killing, by whatever means it is carried out, of a human being in the initial phase of his or her existence, extending from conception to birth) is never permitted”. Obviously this strictly prohibits abortion, but it also provides a clause demonstrating the church’s belief a child becomes human at the point of conception, a distinction many disagree on. Beyond this, directive 52 shows how the church is also against contraception stating, “Catholic health institutions may not promote or condone contraceptive practices”. But what if a couple wants to have a child but one of the two struggle with infertility? To my surprise, directive 40 clearly states that, “Heterologous fertilization is prohibited because it is contrary to the covenant of marriage”. Heterologous fertilization is a type of assisted fertilization in which third party gametes (aka eggs or sperm) are used in the process of fertilization. However the church wants to protect this “covenant of marriage” between the couple, which includes not preventing conception of a child, not aborting a fetus, and having that child come from the husband and wife of a marriage. After all of this, it’s barely a surprise that the church places a ban on gender affirming care. However, the wording is deceptively innocent. What directive 29 really says is, “Catholic health care services and providers ‘must employ all appropriate resources to mitigate the suffering of those who experience gender incongruence or gender dysphoria’ and to provide for the full range of their health care needs, employing only those means that respect the fundamental order of the human body.” So while it seems great that the church acknowledges and wants to provide comfort to those seeking gender affirming care, the clause at the end gives the impression that there is a “correct” and “natural” order to the human body that must be followed, and denies the need for actual gender affirming care at all.
So can this really affect modern day hospitals and residency programs? The short answer is, yes. According to the National Library of Medicine, 1 in 14 obstetrician-gynecologists in the US have graduated from Catholic sponsored institutions where they received their training. The tricky thing about these institutions is that in addition to the ERDs, they must also follow the program requirements set by the Accreditation Council for Graduate Medical Education. Such program requirements offer insight into abortion training, stating “Programs must provide clinical experience or access to clinical experience in the provision of abortions as part of the planned curriculum.” There is also a requirement that states, ““Residents must have didactic activities and clinical experience in all forms of contraception,” which also contradicts the ERDs being sent out to Catholic institutions.
And here is where we get to the real conflict between these two sets of rules in Catholic medical care. The lists directly contradict each other, making it impossible for both of them to be followed earnestly. So because of this, Catholic medical education institutions have two options. The first of which is one that does happen in some programs, which is to do their best to bend the rules and follow all orders the best that they can. For example, some programs may provide simulations of abortion training and implanting contraceptives while not actually having their students perform those procedures in the field, which at least gives them some idea of the operations. However, the downside to this option is that the training provided is suboptimal at best and doesn’t give the students any real-world practical experience. And on the other side of things, it’s working off of a bit of a technicality in the ERDs and could be seen as breaking them.
This is realistically not an issue most institutions have to worry about, however, as the second option of dealing with these rule contradictions is to accept that noncompliance with one of the lists is inevitable. And unfortunately, the ERDs are typically the side that gets seen as more valuable. As a result, residents coming out of these programs have reported dissatisfaction with certain aspects of their education, such as gynecologists never having performed a postpartum sterilization before graduation, which is considered a routine procedure. All of this leads to even more problems when students are hired by hospitals and the tensions between those hospitals and their employees grow.
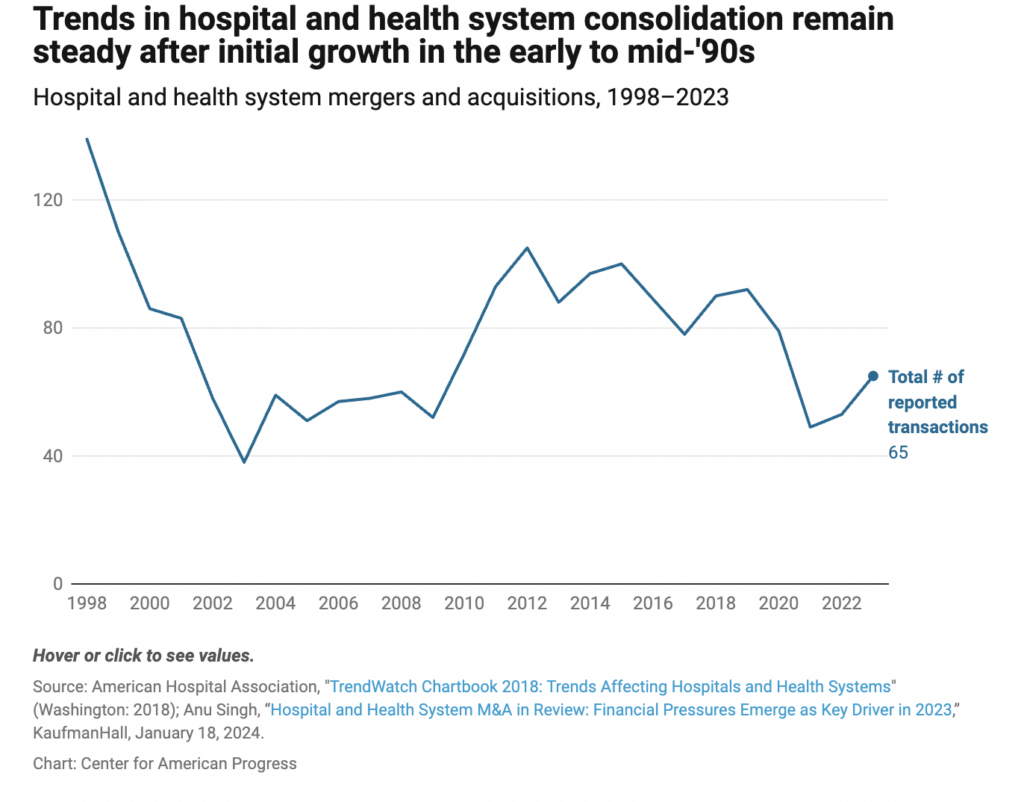
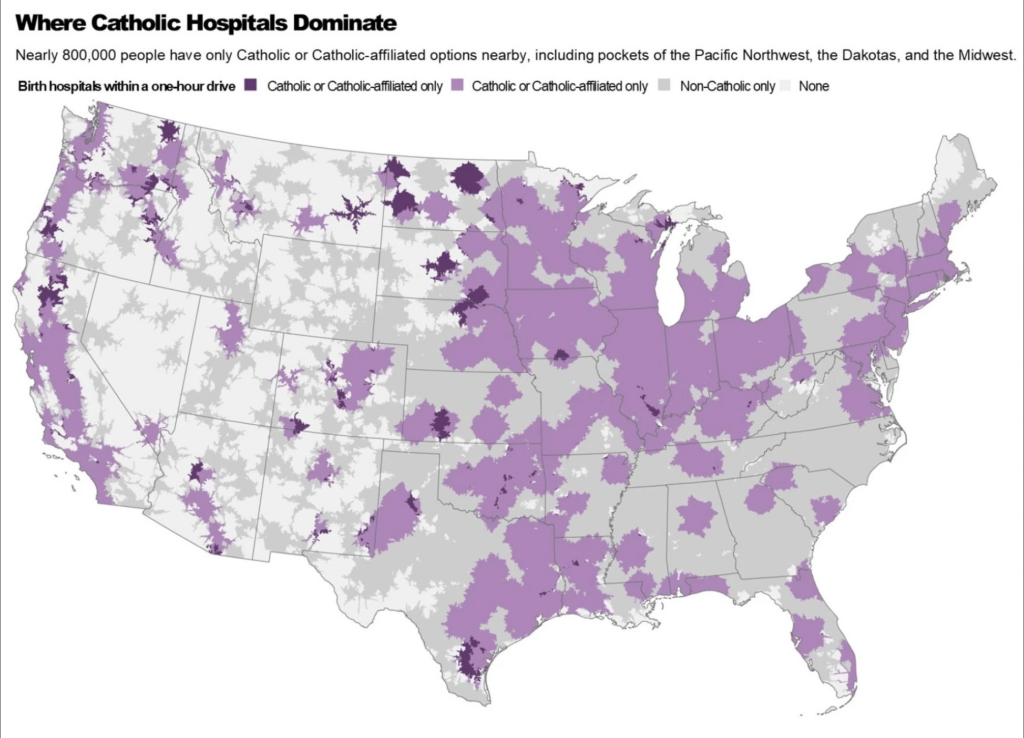
Recently, more and more hospitals are merging or being acquired by large Catholic hospital systems. By 2020, 4 of the 10 largest hospital systems were catholic and 1 in 6 hospital beds in the US were in those catholic hospitals. The problem here is how limited reproductive healthcare becomes as hospitals become acquired by Catholic systems. This is an issue beyond abortion bans in states, as even states where abortion is legal ERDs can cause restrictions. And with Catholic hospital systems growing, this is becoming an increasingly alarming issue.
From here on out, we start to get into the personal, real world impacts all of these larger problems have, starting with their impact on patients. According to the Center for American Progress, “Roughly 1 in 5 Catholic hospitals in the United States do not explicitly disclose their religious affiliation on their websites, and only a small percentage of those disclose how that affiliation might affect patient care.” These hospitals might not see the big deal in disclosing what religion they were originally founded on, but it can have a huge impact on what healthcare patients can or cannot receive, especially when those patients are kept unaware. For example:
Say there is a patient who is having a miscarriage, and they go to the nearest hospital unaware of its religious affiliation because it was in no way disclosed to them. In general, there are a few treatment options for miscarriages. One is to be treated through “expectant miscarriage,” essentially waiting for the body to complete the miscarriage on its own. But for particularly long or painful miscarriages medication such as misoprostol can be administered to speed up the process or in some cases surgical removal of the fetus is best. This patient upon their arrival requests to elicit the help of misoprostol to speed up the process. But only then is it then brought to their attention the Catholic affiliation the hospital has, and that they can only offer them supervised expectant miscarriage care, because it would be against the ERDs to administer either of the two other options. Because of this, many patients can go on to develop infections or risk a complicated and painful transfer to another hospital, with no way of knowing if the new hospital they’re transferring to is Catholic-affiliated because they can’t even look it up on the hospital’s website.
Patients aren’t the only ones negatively affected by these tensions. Many medical employees experience conflicts between their ethical and professional beliefs when employed at Catholic hospitals. A survey taken across 2008-2009 found that more than half of OB-GYNs practicing in catholic hospitals felt conflicted in their place of work because of religious based protocols. One such frustrated medical worker is Lisa Watson. Watson is a registered nurse at Ascension Via Christi St. Francis in Wichita, Kansas. Despite having been registered for almost 20 years, she published an article in Ms. Magazine in 2024 describing her conflicting personal morals and professional beliefs. She mentions how she was drawn to Ascension because of its clear mission of “providing care to all people, and particularly to community members in need.” However she expresses how in her time there, there has been a stark difference between the mission and what actually occurs inside the hospital walls. For some background, Ascension is one of the largest and wealthiest non profit and Catholic hospital systems in the US. Despite this, it also cut one quarter of its labor and delivery units in the last decade. These devastating cuts have led to higher infant mortality rates, and the closures have been more likely to occur in lower income areas, often affecting black and latina patients while preserving the healthcare of white patients. In response to questions about the closures, Ascension has claimed that the reason for the cuts is so they can “consolidate services” to provide more “comprehensive” care. But Watson refutes this statement, for as she puts it, “‘Consolidation’ is not a soothing reassurance for families who need reliable, nearby care.” Ascension is one of the largest healthcare providers in Indiana. But because of these closures, obstetrics deserts have been created to where it is extremely difficult to get proper reproductive care and has led to Indiana having some of the highest rates of pregnancy-related mortality in the country. And when an infant is successfully born, if that child needs any sort of care, even down to the simplest surgeries, some of those infants have been sent as far away as 200 miles because of the lack of resources in these labor and delivery units. And while Ascension will take care of getting the child to the hospital it needs to be at, they force the parents to arrange their own transportation to see their newborn. As mentioned earlier, Ascension has the money to improve the obstetrics conditions in their hospitals. Their leadership simply needs to be pushed to act upon the demands being made by their employees and patients alike.
Thank you for tuning into today’s podcast episode: Directives and Decisions: Conflicting Medical Guidelines in Catholic Healthcare Systems. Today’s topics of conversation are a very small window into the complicated world of religion, medical practices, and reproductive healthcare. But hopefully this gave you the information needed to go out and educate others on this issue and bring some reproductive justice onto this large issue in US hospitals. Bye for now!

References
ACGME program requirements for graduate medical education in, September 3, 2025. https://www.acgme.org/globalassets/pfassets/programrequirements/2025-reformatted-requirements/220_obstetricsgynecology_2025_reformatted.pdf.
Devin Blake. “Ascension to Close South Side Milwaukee’s Only Labor and Delivery Unit, Prompting Questions and Protest.” Wisconsin Watch, April 25, 2024. https://wisconsinwatch.org/2022/12/ascension-to-close-south-side-milwaukees-only-labor-and-delivery-unit-prompting-questions-and-protest/.
“History.” Catholic Health Association of the United States. Accessed November 20, 2025. https://www.chausa.org/about/our-association/history.
Rachana Pradhan. “The Powerful Constraints on Medical Care in Catholic Hospitals Across America.” WUSF, February 24, 2024. https://www.wusf.org/health-news-florida/2024-02-24/the-powerful-constraints-on-medical-care-in-catholic-hospitals-across-america.
Sanders, Bailey, Barak Richman, and Kierra B. Jones. “Growing Market Power among Catholic Hospitals Restrains Access to Reproductive Health Care – Center for American Progress.” Center for American Progress, September 29, 2025. https://www.americanprogress.org/article/growing-market-power-among-catholic-hospitals-restrains-access-to-reproductive-health-care/.
Smith, James F. “Should Catholic Academic Health Centers Sponsor Residency Training in Obstetrics and Gynecology?” Journal of graduate medical education, December 2019. https://pmc.ncbi.nlm.nih.gov/articles/PMC6919164/.
Sybert, Christine. “The ERDS: Part One – the Social Mission of Catholic Health Care Services.” The Linacre quarterly, November 2021. https://pmc.ncbi.nlm.nih.gov/articles/PMC8689497/.
United States Conference of Catholic Bishops. Ethical and religious directives for Catholic Health Care Services, November 2025. https://www.usccb.org/resources/ERDs-7th-ed-Approved_2025-11-12.pdf.
Watson, Lisa. “We Must Stop Catholic Hospitals from Closing More Labor and Delivery Units.” Ms. Magazine, May 13, 2024. https://msmagazine.com/2024/05/10/ascension-catholic-hospital-labor-delivery-health-birth-mother/.


