Hanlan Paquin
Transcript
Hello, hello, hello, and welcome back!! I am your host, Hanlan, and today we are going to be dipping our toes into the world of IUDs. So without further ado, let’s head straight into it!
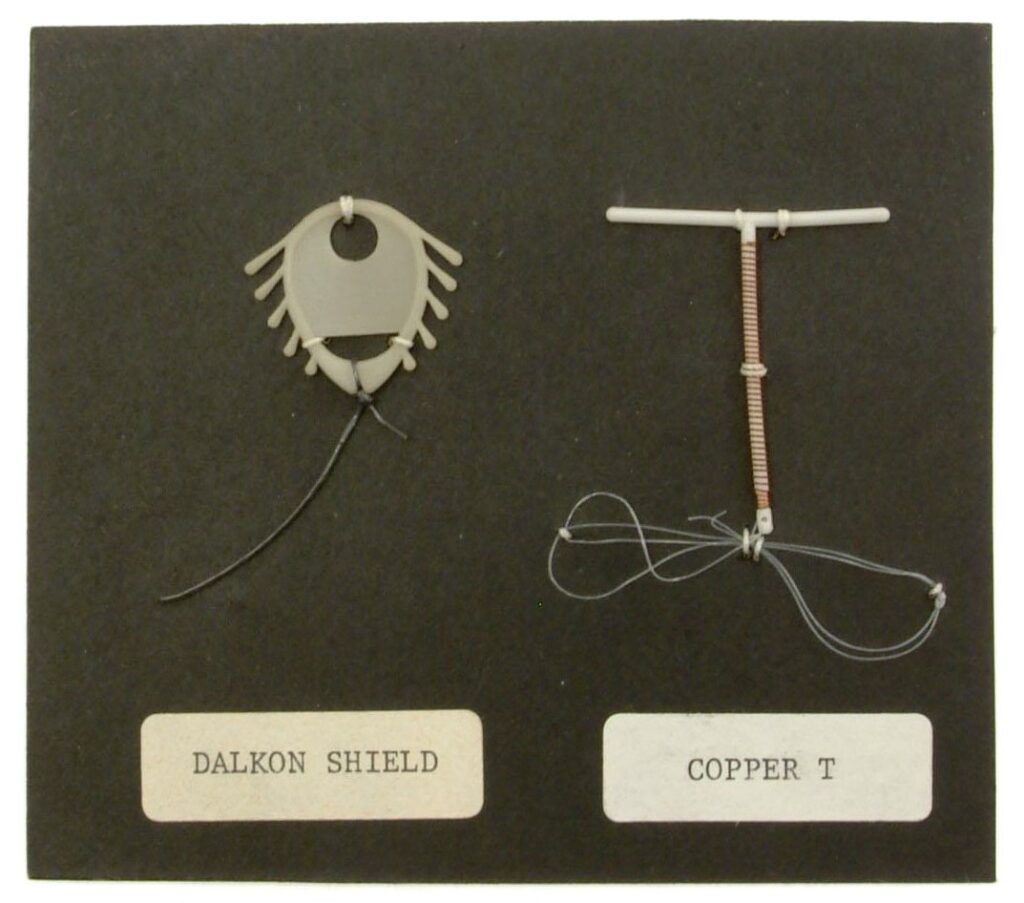
IUD stands for intrauterine device. They are small “T” shaped plastic devices for birth control that are inserted into the uterus, with the “T” shape allowing them to not fall out. There are two types of IUDs- hormonal, and copper. Hormonal IUDs release a small amount of progestin- about 20 micrograms, which is a synthetic form of progesterone, every 24 hours.1 This progestin dose thickens cervical mucus to keep sperm from entering the uterus, and thins the uterine lining, making it difficult for an ovum, or an egg, to implant itself in the uterus if it were to become fertilized. Copper IUDs have a small copper wire wrapped around the base of the “T” which works to make the uterus a hostile environment for sperm, as the copper repels it, making it impossible for the sperm to fertilize the ovum.2 The main function of an IUD is birth control, but some women get them inserted to mitigate period pains, as some types of IUD may lessen cramps, reduce bleeding, and even stop periods altogether, though this depends on the type of IUD and the person it’s inserted into.3
The first IUD dates back to a design made by Dr. Richard Richter in 1909 and was made from silk worm guts. In the 1920s, a German doctor, Ernst Grafenberg created a ring shaped IUD utilizing metal alloys, and reported a less than 1% pregnancy rate among women using them.4 And in the 1970s, a new type of IUD emerged.
Loretta Ross: “The Dalkon Shield was an intrauterine device manufactured by A.H. Robins, a little triangular piece of plastic with little edges on it. It was put up against the cervix to block sperm getting to the uterus. But it did have a design flaw in that it had a string hanging down from it that was literally there only to aid the doctor in removing it. That’s all it was there for. It was like a wick on a candle. Well, it also acted like a wick, because it allowed bacteria to wick up that string into one’s uterus.”5
By 1970, 10% of women on birth control in the United States had an IUD, however the Dalkon Shield began causing issues for patients. By 1985, twenty-one women had died, and 13,000 were infertile or sterile as a result of infection like pelvic inflammatory disease transmitted through the string of the IUD and into the women’s uterus, as the string wasn’t sealed on either side to prevent bacteria from traveling upwards.6
Nowadays there are several IUDs on the market, and they are the third most used birth control in the United States, after the birth control pill and tubal litigation. In the United States there are five FDA approved IUDs, four hormonal, and one copper; Mirena and Liletta which last up to eight years, Kyleena, which lasts five years, Skyla, lasting three, and the Paragard copper IUD, which lasts for up to ten years.7
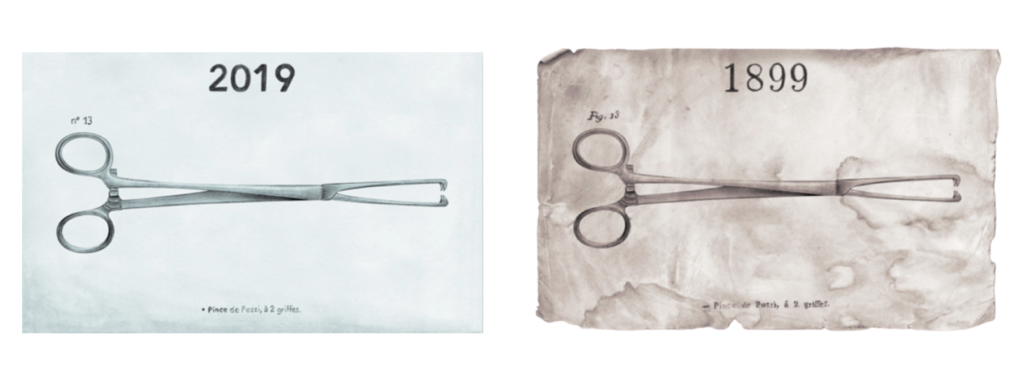
IUD insertions take about 5 to 15 minutes, and utilize a couple different gynecological tools. Some of these tools include the speculum, the IUD insertion tube, and the tenaculum. Now, tenaculums originated during the American Civil War, and were originally used to remove bullets from gunshot wounds by surgeons on the field or to pull arteries out in order to tie them off so that patients didn’t bleed out. A tenaculum looks like a pair of scissors with two sharp hooks on the end, and to access the uterus during IUD insertions, gynecologists will insert the tenaculum into the vagina while the speculum opens the vagina open, and using the sharp hooks on the end the tenaculum they will pierce the cervix to give the doctor a firm hold of the cervix. The use of the tenaculum often causes intense pain, cramping, and bleeding. 8
Patient 1: When I got my IUD inserted they told me the pain was going to be a firm pinch for a few seconds, I wasn’t expecting to feel a searing pain and to nearly lose consciousness on the table, but I did” Alternatives to tenaculums
In March of 2020 one 16 year old patient got her IUD inserted:
Patient 2: I lie down. I’m like “so there really isn’t any way that we can numb anything or you know, like any anesthesia?” and she was like “No, science hasn’t come that far yet.” They gave me two Tylenol and I laid back and yeah, you see white for a second with them clamping on to your cervix. Everyone that had told me that had an IUD was like it’s like the worst period cramp you’ve ever had and I’m like okay, I can wrap my head around that pain. She takes it out, but that, that pain is not- you know it’s not quite hot, but oh it’s bad. So I’m kind of sweating and I feel my hands are getting clammy, but whatever, I just gotta make it to the car. I open the car door and I sit down and my mom goes “So how to go?” and I just lean over and puke all over the parking lot and the worst part was I just remember the visual of seeing myself throw up the two Tylenol that I took, and we didn’t take any Tylenol with me. So I wasn’t gonna feel any relief for the next 30 minutes at least on the car ride home. My mom called and was like “Hey, like I’m concerned” and they were like “Oh no it’s raining like don’t worry about it.” My mom was like “Well no, no about your fucking parking lot. I was worried that if she should be throwing up” and they’re like “Yeah that’s normal.”
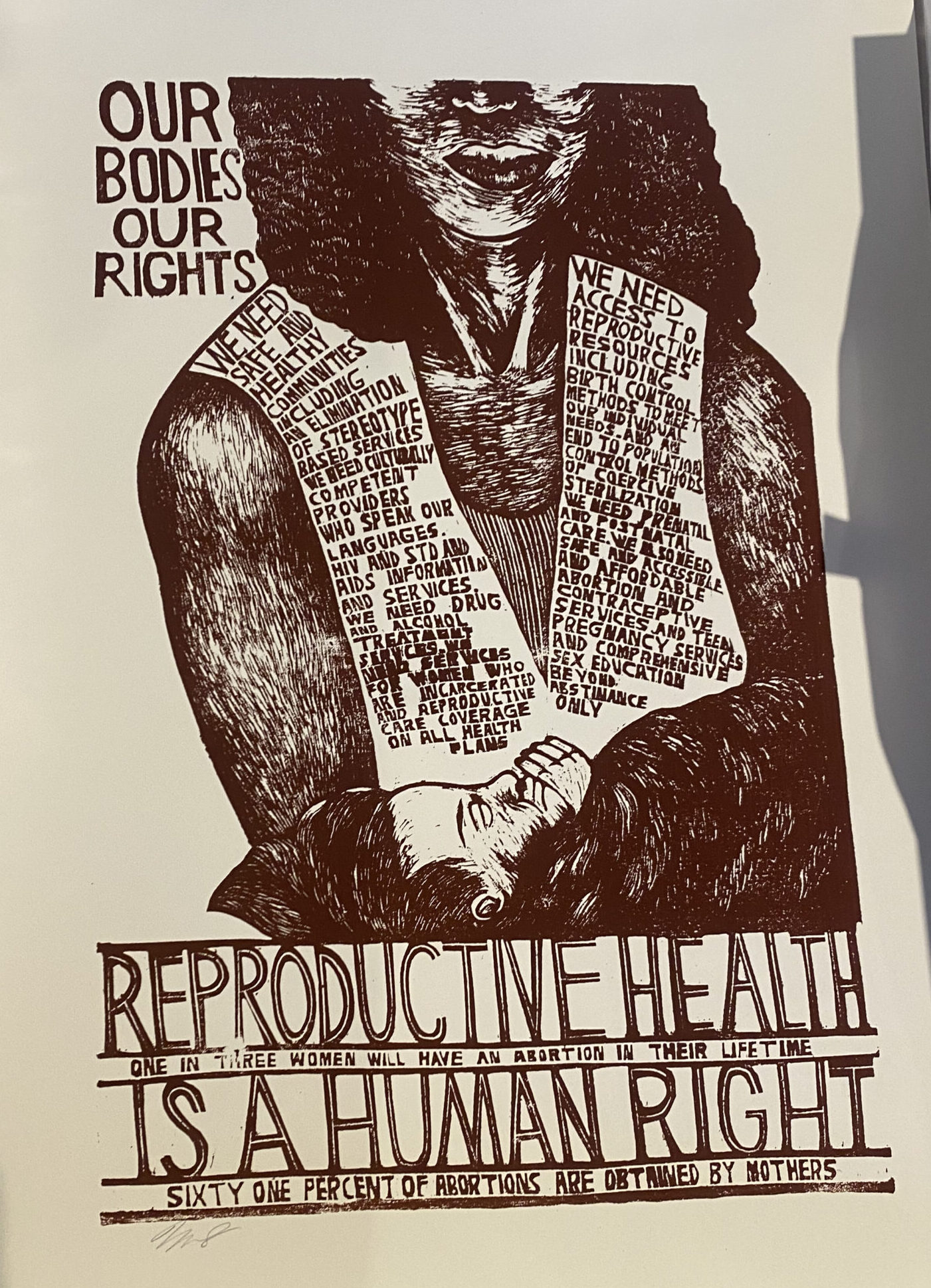
The lack of personalized or attentive care and pain management for the patient is appalling, and quite frankly, is an all too common experience for people seeking IUDs. This experience is clearly indicative of a need for better pain management support for IUD insertions, though there would be no change in care for over five years.
On November 19th, 2024, the CDC released new recommendations for intrauterine contraception insertions after evidence from a study suggested that topical anesthetics may reduce patient pain. These new recommendations indicate that using lidocaine- either topical or injected as a paracervical block may make IUD insertion significantly less painful for patients.9 In May of 2025, the American College of Obstetricians and Gynecologists released new recommendations for IUD insertion pain management. The chief of clinical practice and health equity and quality believes that these new recommendations are essential to create “comprehensive pain management counseling—not just for mitigating pain in the moment but also for improving trust with our patients and ensuring better access to gynecologic health care for every person.”10 These recommendations include the use of lidocaine spray, lidocaine-prolocaine cream, or a paracervical block to reduce pain involved with insertion. While a limited number of practitioners did offer pain management treatments like topical lidocaine prior to these new recommendations, the new CDC and American College of Obstetricians and Gynecologists guidelines will ensure that even more women can receive this pain management treatment with their IUD procedures; making gynecological care more accessible to everyone.
- Hubacher, David. “The Checkered History and Bright Future of Intrauterine Contraception In the United States.” Perspectives on Sexual and Reproductive Health 34 (March 1, 2002): 98–103. https://www.guttmacher.org/journals/psrh/2002/03/checkered-history-and-bright-future-intrauterine-contraception-united-states. ↩︎
- “How Does an IUD Work?: New England Women’s Healthcare: OBGYNs.” Accessed December 4, 2025. https://www.newh-obgyn.com/blog/how-does-an-iud-work. ↩︎
- Family Planning Tasmania. “Factsheet Resource List,” April 5, 2023. https://fpt.org.au/advice-and-information/factsheets-resources/. ↩︎
- https://muvs.org/en/museum/newsletter/2006-12-05-december-2006/
↩︎ - Loretta Ross interview by Joyce Follet, video recording,
November 3, 2004, Voices of Feminism Oral History Project, Sophia Smith Collection,
tape 2. ↩︎ - “The Troubled History of the IUD | Adyn,” accessed December 4, 2025, https://adyn.com/blog/iud-history/. ↩︎
- “What Women Should Know About Intrauterine Devices (IUDs),” Yale Medicine, accessed December 4, 2025, https://www.yalemedicine.org/news/intrauterine-devices-iud. ↩︎
- Aspivix, “Tenaculum: For Over 100 Years Women Have Endured Pain in Gynecology,” Aspivix, October 28, 2020, https://www.aspivix.com/tenaculum-for-over-100-years-women-have-endured-pain-in-gynecology/. ↩︎
- CDC, “Intrauterine Contraception,” Contraception, November 19, 2024, https://www.cdc.gov/contraception/hcp/usspr/intrauterine-contraception.html. ↩︎
- “ACOG Releases New Recommendations on Pain Management for IUD Insertions, Other In-Office Gynecologic Procedures,” accessed December 4, 2025, https://www.acog.org/news/news-releases/2025/05/acog-releases-new-recommendations-on-pain-management-for-iud-insertions-other-in-office-gynecologic-procedures. ↩︎